COVID-19 VACCINATION
Vaccination is strongly encouraged for everyone ages 5 and older. Call Nimiipuu Health at 208-843-2271 (Lapwai) or 208-935-0733 (Kamiah) to schedule your appointment. Vaccinations at Nimiipuu Health are available to anyone, beneficiary or not.
NPT is at a Medium Risk Level
The Nez Perce Tribe is considered to be at the medium level, based on CDC’s scale. The Nez Perce Tribe will retain the requirement of unvaccinated individuals to wear a mask while indoors in shared spaces. Nimiipuu Health will continue to monitor numbers to determine the Nez Perce Tribe’s risk level and notice will be sent for any changes.
NPT Following STAGE 4 Protocols
The Nez Perce Tribe is currently following the protocols of Stage 4 of the Idaho Rebounds guidelines. Stage 4 allows for large gatherings/events and continued travel. Social distancing must continue where possible. Regular sanitation and hand washing is a must.
For events, every attempt should be made to host outdoors. If this is not feasible, event planners should aim for a venue with enough space to comfortably fit the desired attendance size with six-foot distancing, high ceilings and good ventilation. If a person feels sick, they are required to stay home and monitor symptoms.
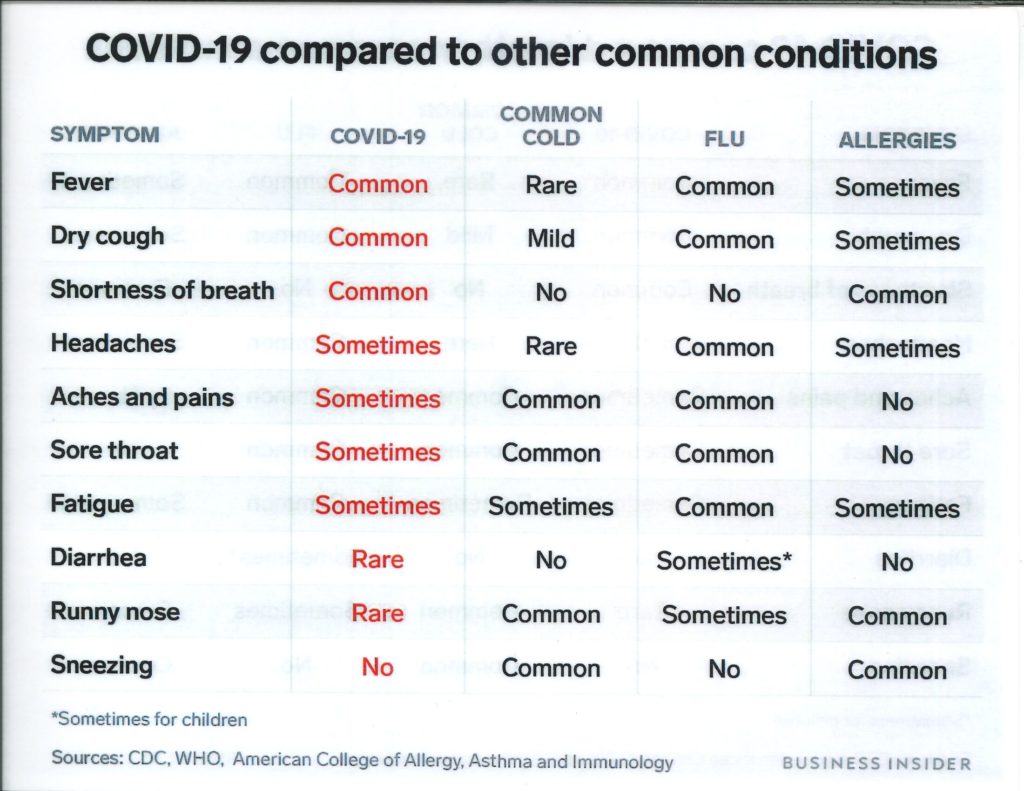
COVID-19 testing is encouraged should aligning symptoms appear.
COVID-19 Vaccine:
When You’ve Been Fully Vaccinated
When You’ve Been Fully Vaccinated -video
Understanding mRNA COVID-19 Vaccines
Janssen (Johnson & Johnson) Vaccine Information
Additional Janssen Vaccine Questions Answered
Coronavirus: What You Need to Know
Organizational Updates:
Nez Perce Tribe – COVID-19 Update Log
Questions? Safety Concerns? Email: nptemergencyoperations@nezperce.org
CRITFC: Safe Fishers, Safe Fisheries
Video Addresses:
June 25, 2021- NMPH Provider Update
March 11, 2021- Janssen (Johnson&Johnson) Vaccine
February 23, 2021- COVID-19 Vaccine Q&A
January 29, 2021- Pandemic Response Update
December 23, 2020- Understanding the COVID-19 Vaccine
November 10, 2020- COVID-19 Update From Dr. Hartwig
October 13, 2020- Update and Information during COVID-19 Pandemic
August 28, 2020- FAQ With Dr. Hartwig
August 20, 2020- A Message from NPTEC
July 30, 2020- Updates from Chairman Wheeler & Dr. Hartwig
June 25, 2020- COVID-19 Update and Recommendations from Dr. Hartwig
June 5, 2020- Public Address by NPTEC Chairman, Shannon Wheeler
April 29, 2020 – NPTEC Chairman Wheeler
April 2, 2020 – NMPH Medical Director, Dr. Kim Hartwig
March 27, 2020 – NPTEC Chairman Wheeler & Incident Commander Antone
March 18, 2020 – NPTEC Chairman Wheeler
Center for Disease Control:
Idaho Rebounds: Guidelines for Opening Up Idaho
Printables
Keep the Distance of an saq’antáayx Wing Span
COVID-19 Frequently Asked Questions (FAQs)
Written by Dr. Hailey Wilson, Nez Perce Tribal member
Disclaimer: Dr. Wilson is not a COVID-19 expert; most information provided is from the Center for Disease Control and Prevention (CDC) website
1) I saw a family member in the store the other day and then they later came back positive for COVID-19, was I exposed?
According to the CDC the definition of exposure or close contact is:
- Within 6 feet of someone with COVID-19 for 15 minutes or longer
- Providing care at home to someone who is sick with COVID-19
- Direct physical contact such as hugging or kissing
- Sharing eating or drinking utensils
- That person sneezed, coughed or somehow got respiratory droplets on you
2) What should I do if/when I am exposed or come in close contact with a COVID-19 positive person?
Stay home and monitor your health
- Stay home/quarantine for 14 days after your last contact with that person
- Watch for fever (>100.4F), cough, shortness of breath, or other symptoms of COVID-19 (updated list also includes: fatigue, body aches, headache, loss of taste or smell, sore throat, nausea or vomiting, diarrhea)
- If possible, stay away from others in your household, especially people who are at higher risk for severe illness
- It is also helpful to contact those individuals you may have exposed. We know that contact tracing is helpful but sometimes there are delays as NMPH and the health department are working very hard to control the spread
If you have already recovered from COVID-19 infection and come into close contact with a positive person or develop new symptoms, you should isolate yourself and contact your healthcare provider about evaluation and possible re-testing, unless it has been less than 3 months since your infection. Then you don’t need to quarantine or re-test.
3) How do I isolate or quarantine if I am homeless or live in a house with other family members who are not sick or who are high risk?
The Nez Perce Tribe has agreements with local hotels and RV sites that can help accommodate isolation and quarantine. If this is needed, contact Nimiipuu Health (NMPH) or the emergency operations center (EOC).
4) My coronavirus test came back positive; do I need to go to the clinic or the hospital?
If you are very sick with trouble breathing or other emergency symptoms (see next question) go to the emergency room or call 911.
Most people will not need in clinic or hospital medical care for their COVID-19 illness. If you are positive with COVID-19:
- Stay home except to get medical care; DO NOT go out to public places. If you need supplies, medications or groceries, ask a family member or friend that is not positive AND does not live in your household
- Take care of yourself. Get rest, stay hydrated, take over the counter medications such as Tylenol or ibuprofen to help you feel better
- Having a poor appetite and low food intake can be normal; you do not need to force yourself to eat. You should however, make sure you are taking in plenty of fluids (water, juice, sports drinks, soup, pedialyte, popsicles, etc.) to avoid dehydration
- As much as able, stay in one specific room away from others and if able use a separate bathroom. If you need to be around others in your household, wear a mask
- Wear a mask over your mouth and nose, cover your coughs and sneezes, clean your hands often, avoid touching your face, avoid sharing personal items, and clean all high touch surfaces everyday (phone, remote controls, counters, tabletops, doorknobs, bathroom fixtures, toilets, keyboards, tablets, bedside tables)
Many people’s symptoms and illness can get worse around days 7-10 of illness, make sure to have the medications you need and a pulse oximeter during this time.
5) When should I seek medical attention for my COVID-19 infection?
If you have any of these emergency warning signs go to the emergency room or call 911:
- trouble breathing
- persistent pain or pressure in chest
- new confusion
- inability to wake or stay wake
- bluish lips or face
- oxygen levels are <90% at rest OR after walking (see next question regarding pulse oximeter)
6) My family member offered to buy me supplies while I’m in isolation/quarantine due to COVID-19 infection, what should I tell them to get me?
It is encouraged to put a table outside your house so that people can easily drop items off for you.
- Water and electrolyte drinks such as Gatorade or Pedialyte
- Pain and fever reducing medications such as Tylenol/acetaminophen or Motrin/ibuprofen
- These medications are safe to use in combination if needed, please follow the dosing guidelines on the package or from your medical provider
- If you have questions about the medications that are safe for you, please consult your medical provider, dosing may be different for people with kidney or liver disease or may be not safe for some, such as for people who have a history of a bleeding ulcer.
- Cough medications: cough drops, Mucinex, Robitussin, or antihistamines such as Benadryl/diphenhydramine or Zyrtec/cetirizine
- A pulse oximeter (device that can measure your heart rate and oxygen levels); Nimiipuu Health may also have devices that they can loan out to positive individuals
- Cleaning supplies
- Necessary groceries
7) When does my quarantine or home-isolation end?
You can stop your isolation or quarantine:
- ISOLATION: 10 days after your symptoms first appeared (or your positive test) AND 24 hours without fever (without using fever-reducing medications) AND other symptoms are improving (some symptoms such as cough and change in taste or smell can persistent much longer).
- QUARANTINE: If you were exposed/close contact you should stay home for 14 days after your last exposure to the positive person (unless you have already had COVID-19 infection and recovered within the last 3 months, then you don’t have to quarantine)
8) Do I need to get retested before I go back to work or school or get out of quarantine?
No, after you are done with your isolation or quarantine (as guided above) you do not need to get retested. This can contribute to a shortage of testing resources that are needed for other people. Some people can still have a positive test for weeks after they have recovered but they are no longer thought to be contagious.
9) How is coronavirus spread? Can I get it from my packages in the mail or by going into a sweathouse? What about going to the store?
The virus is spread by respiratory droplets that are produced by an infected person when they cough, sneeze or talk. These droplets can then land in mouths or noses of people nearby or land on our hands and we bring those droplets to our face when we touch our face. The virus can survive for a short time on some surfaces. It is unlikely to be spread from mail or packages. Wear a mask, wash your hands often and avoid touching your face. It is also encouraged to sanitize shopping carts prior to use, spending minimal time in stores and avoid touching a lot of surfaces if you can.
If you are in close contact with a person who is positive in a sweathouse, the virus can be spread that way (see question 1 for definition of exposure). It is encouraged to only sweat with other members of your household. The virus is not thought to be shed through normal sweat glands, so going sweat AFTER a person who is positive is highly unlikely to spread the virus.
10) I’ve been very lonely, worried, or depressed, is this normal?
Pandemics are very stressful! There have been significant increases in mental health issues across the nation, you are not alone.
- Many are feeling lonely and isolated
- Some people have increased levels of stress due to loss of employment or other income sources, children being out of school or needing to be homeschooled, lack of childcare
- Many have fear and anxiety about getting infected or are worried about high risk family members getting infected
Here are some mental health resources:
- If you are in crisis and need immediate help, call 911
- Disaster distress helpline: 1-800-985-5990
- National Suicide Prevention Lifeline: 1-800-273- TALK (8255)
- National Domestic Violence Hotline: 1-800-799-7233 or text “LOVEIS” to 22522
- National Child Abuse Hotline: 1-800-4ACHILD (422-4453) or text 1-800-422-4453
- National Sexual Abuse Hotline: 1-800-656-HOPE (4573)
- The Eldercare Locator: 1-800-677-1116
- Veteran’s Crisis Line: 1-800-273-TALK (8255) or text 8388255
- Substance abuse help, SAMHSA’s National Helpline: 1-800-662-HELP (4257)
- Nez Perce Tribe’s Women’s Outreach Program “Úuyit Kímti Program”: 855-803-4685
- Nimiipuu Health (medical and mental health): 208-843-2271
Other tips to help with your mental health
- Check in with your family members and elders via phone, text or social media
- Take care of your emotional and physical health:
- get regular sleep
- eat healthy and well-balanced meals
- take breaks from watching, reading or listening to the news
- take deep breaths, stretch or meditate (there are many free YouTube videos and free smart phone apps)
- exercise regularly, it is safe to be outside exercising during the pandemic (remain distanced from others)
- avoid excess alcohol and drug use
- take time to unwind, do activities that you enjoy
- connect with others
- Knowing the facts about COVID-19 and stopping the spread of rumors can help reduce stress and stigma.
- The CDC website is a great resource: CDC.gov/coronavirus
- If you are already on medications for mental health conditions, continue taking your medications regularly and checking in with your mental health provider.
11) I had a negative COVID-19 test, am I ok to be out in the community?
If you have been in close contact/exposed to someone with COVID-19, you should remain in quarantine for 14 after your last contact with that person. No lab test is perfect and there also needs to be enough time between exposure and your test for the virus to build up in your body to turn the test positive. You may have the infection but it may be too early to get a positive result.
12) I already had COVID-19, can I get it again?
There is a lot that is still unknown about COVID-19 infection including whether or not people who have recovered remain immune to the illness. It is unknown if you can get infected again.
13) How will the COVID-19 infection affect my body in the long term?
Most people recover from this illness without any long-term consequences or symptoms however some people may develop long term issues. For people who had severe respiratory infection due to COVID-19, there can be scarring and other changes within the lungs which may lead to chronic lung problems. There can also be an increased risk of blood clots in the setting of COVID-19 infection including strokes, which can potentially cause long term neurological deficits. But strokes are not common.
14) Who is high risk for COVID-19 infection?
People of any age with the following conditions are at increased risk for severe illness:
- Cancer
- Chronic kidney disease or CKD
- Chronic obstructive pulmonary disease or COPD or emphysema
- Immunocompromised state (weakened immune system) from solid organ transplant
- Obesity, BMI 30 or higher
- Serious heart conditions: heart failure, coronary artery disease/prior heart attack or cardiomyopathies
- Type 2 Diabetes Mellitus
People with the following conditions might be at an increased risk of severe infection:
- Asthma
- Cerebrovascular/brain disease: prior stroke
- Cystic fibrosis
- High blood pressure
- Neurologic conditions such as dementia
- Liver disease
- Pregnancy
- Pulmonary fibrosis
- Smoking
- Type 1 Diabetes Mellitus
- Immunocompromised state from blood or bone marrow transplant, immune deficiencies, HIV, chronic corticosteroid use or other immune weakening medications
15) Are there vitamins or supplements that I can take the help prevent me from getting sick?
There have not been any good studies to indicate any specific vitamin or supplement to treat or prevent COVID-19 infection. Also keep in mind that supplements are not regulated by the FDA, so there is no way of knowing for sure what is actually in the vitamins and supplements that are bought over the counter.
- Vitamin D: There have been prior studies that show people with low vitamin D levels may have worse respiratory infections. You can get vitamin D in food (fortified dairy products and cereals and fatty fish) and with direct sunlight exposure (avoid burning or sun tanning). There are also over the counter vitamin D supplements. There are studies being done now for vitamin D and COVID-19 infection.
- Zinc: Zinc is known to play a role in our immune function, it helps our body make white blood cells and antibodies (infection fighting cells). High dose zinc has been shown to help reduce symptoms of common cold but its role in COVID-19 infection is not clear at this time and is currently being studied.
- Vitamin C: Acts as an antioxidant and some studies have shown that it can help our immune system (infection fighting system). Clinical trials are being done now to determine if vitamin C might be helpful in COVID-19 infection.
16) Am I going to have to be on a breathing machine if I go to the hospital?
The majority of people that get sick from COVID-19 will not need oxygen or need to be on a breathing machine. However, COVID-19 infection does increase the risk for both of these. Medical providers will likely do everything they can before placing you on a breathing machine.
If you DO NOT wish to be put on a breathing machine, please talk with your family members early about these wishes… These are very difficult but very important conversations to have and it is best to have them before you get sick and are in a serious health situation.
17) What if my kid gets sick?
There is not much different to do when children get sick compared to adults. Make sure to have medications for them available, as well in the appropriate doses. Make sure they are drinking enough fluids to stay hydrated (peeing normally, lips and skin are not dry). If they have high fevers over many days, are working hard to breathe or any of the items listed in question 5 seek emergency care.
For infant 2 months old or young, having a fever >100F, go to the emergency room.
The best ways to prevent the spread of COVID-19 and to protect our families and our Tribe are to continue social distancing (remain at least 6 feet away from other people), wear a mask whenever you are out of your house and in potential contact with others, hand/sanitize your hands frequently, avoid touching your face, avoid groups/crowds of more than 10 people.